What is Urinary System?
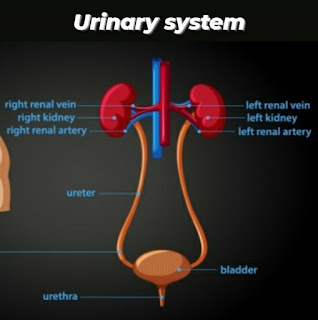
The Urinary system is the main excretory system and consists of the following structures:
1- kidneys - which secrete urine
2- Ureters - that convey the urine from the kidney to the urinary bladder.
3- Urinary bladder - which collects and stores urine.
4- Urethra - urine leaves the body.
Kidneys :
The kidneys lie on the posterior abdominal wall, one on each side of the vertebral column, behind the peritoneum and below the diaphragm. They extend from the level of the 12th thoracic vertebra to the 3rd lumber vertebra, receiving some protection from the lower rib cage.
Kidneys are bean-shaped organs,it is about 11cm long, 6cm wide, 3cm thick and weight 150g.
Functions of kidney
:
1- formation of urine,maintaining . water,electrolytes and acid-base balance.
2- excretion of waste products.
3- production and secretion of . Erythropoietin of red blood cells.
4- production and secretion of renin, an important enzyme in the control of blood pressure.
Microscopic structures of the kidneys :
The kidneys contains about 1-2 millions functional units, the nephrons and a much smaller number of collecting ducts. The collecting ducts transport urine through the pyramids to the calyces, giving the pyramids their striped appearance.
The Nephron :
The nephrons is essentially a tubule closed at one end that joins a collecting ducts to other end. The closed end is indented to form a cup-shaped glomerular capsule, which almost completely encloses a network of tiny arterial capillaries, the glomerulus. Nephrons is about 3cm long and described in three parttubule
1- the proximal convoluted tubule
2- the medullary loop
3- the distal convoluted tubule
The collecting ducts unite, forming larger ducts that empty into the minor calyces.
The kidneys receive about 20% of the cardiac output. After entering the kidneys at the hilum, the renal artery divided into smaller arteries and arterioles. In the cortex an arteriole, the afferent arteriole, enters each glomerular capsule and then subdivides into a cluster of tiny arterial capillaries, forming the glomerulus. Between these capillary loops are connective tissue phagocytic mesangial cells, which are part of the monocyte - macrophage defence system. The blood vessels leading away from the glomerulus in the efferent arteriole. The afferent arteriole has a large diameter than the efferent arteriole, which increase pressure inside the glomerulus and drives filtration across the glomerular capillary walls. The efferent arteriole divides into a second peritubular capillary network. This maintains the local supply of oxygen and nutrients and removes waste products. Venous blood drained from this capillary bed eventually leaves the kidney in the renal, which empties into the inferior vena cava.
The walls of the glomerulus and the glomerular capsule consists of a single layer of flattened epithelial cells. The glomerular walls are more permeable than those of other capillaries. The reminder of the nephron and the collecting duct are formed by a single layer of simple squamous epithelium.
Renal blood vessels are supplied by both sympathetic and parasympathetic nerves. The presence of both dividision of the autonomic nervous system controls renal blood vessels diameter and renal blood flow independently of autoregulasecretion
Formation of Urine
The kidneys form urine, which passes to the bladder for storage prior to excretion. The composition of urine reflects exchange of substances between the nephron and the blood in the renal capillaries. Waste products of protein metabolism are excreted, water and electrolyte levels are controlled and PH is maintained by excretion of hydrogen ions. There are three processes involved in the formation of urine.
1- Filtration
2- selective reabsorption
3- secretion
1- Filtration
This takes place through the semipermeable walls of the glomerulus and glomerular capsule. Water and other small molecules readily pass through, although some are reabsorbed later. Blood cells, plasma proteins and other large molecules are too large to filter through and therefore remain in the capillaries. The filtrate in the glomerulus is very similar in composition to plasma with the important exceptions of plasma proteins and blood cells.
Filtrate takes place because there is a difference between the blood pressure in the glomerulus and pressure of the filtrate in the glomerular capsule. Because the efferent arteriole is narrower than the afferent arteriole, a capillary hydrostatic pressure of about 55 mmHg builds made up in glomerulus.
This pressure by the osmotic pressure of the blood, provided mainly by plasma protein, about 30mmHg and by filtrate hydrostatic pressure of about 15mmHg in glomerular capsule. The net filtration pressure is, therefore:
. 55 - (30+15) = 10
The volume of filtrate fromed by both kidneys GFR (Glomerular Filtration Rate). In a healthy adult the GFR is about 125mL/min.
2- Selective reabsorption:
Most reabsorption from the filtrate back into the blood takes place in the proximal convoluted tubule, Many substances are reabsorbed here, including some water, electrolytes and organic nutrients such as glucose. Some reabsorption is passive, but some substance, e.g. glucose, are actively transported. Only 60-70% of filtrate reaches the medullary loop. Much of this, especially water, sodium and chloride, is reabsorption in the loop, so that only 15-20% of the original filtrate is now very different. More electrolytes are reabsorbed here, especially sodium .
Active transport takes place at carrier sites in the epithelial membrane, using chemical energy to transport substances against their concentration gradients.
Some ions, i.e. sodium and chloride, can be absorbed by both active and passive mechanisms depending on the site in the nephron.
3- Tubular secretion:
Filtration occurs as blood flows through the glomerulus substances not required and foreign material, e.g. drugs including penicillin and aspirin, may not be entirely filtered out of the blood because of the short time it remains in the glomerulus. Such substances are cleared by secretion from the peritubular capillaries into the filtrate within the convoluted tubules. Tubular secretion of hydrogen ions is important in maintaining normal blood PH.
Composition of urine:
Urine is clear and amber in colour due to the presence of urobilin, a bile pigment altered in the intestine, reabsorbed then excreted by the kidneys. The specific gravity is between 1020 and 1030, and the PH is around 6. A healthy adult passes from 1000 to 1500 ml per day. The volume of urine produced and the specific gravity vary according to fluid intake and the amount of solute excreted. The constituents of urine are:
Water =96%
Urea = 2%
Uric acid
Creatinine
Ammonia. = 2%
Sodium
Potassium
Chloride
Phosphate. = 2%
Sulphate
Oxalates
Water balance and urine output:
The source of most body water is dietary food and fluid although a small amount is formed by cellular metabolism. Water is excreted as the main constitute of urine, in expired air , faeces and through the skin as sweat. The amount of sweat produced is associated with environmental and body temperature.
Electrolyte balance:
Changes in the concentration of electrolytes in the body fluids may be due to changes in ;
1-) the body water content, or
2-) electrolyte levels
Several mechanisms maintain the balance between water and electrolyte concentration.
Ureters :
The Ureters carry urine from the kidneys to the urinary bladder. They are about 25-30 cm long with a diameter of approximately 3mm. The ureter is continuous with the funnel-shaped renal pelvis. It passes downwards through the abdominal cavity, behind the peritoneum in front of the psoas muscle into the pelvic cavity, and passes obliquely through the posterior wall of the bladder.
Structure:
The walls of the ureters consists of three layer of tissue.
An outer covering of "fibrous tissue", continuous with the fibrous capsule of the kidney.
A middle " muscular layer" consisting of interlacing smooth muscle fibres that form a functional unit round the ureter and an additional outer longitudinal layer in the lower third.
An inner layer, the "mucosa" , composed of transitional epithelium.
Functions :
Peristalsis is an intrinsic property of the smooth muscle layer that people urine along the ureter. Peristaltic waves occur several times per minute, increasing in frequency with the volume of urine produced, sending little spurts of urine along the ureter towards the bladder.
Urinary bladder :
The urinary bladder is a reservoir for urine. It lies in the pelvic cavity and its size and position vary, depending on the volume of urine it contains. When distended , the bladder rises into the abdominal cavity.
Structure:
The bladder is roughly pear shaped , but becomes more balloon shaped as it fills with urine. The posterior surface is the base. The bladder opens into the urethra at its lowest point, the neck.
The peritoneum covers only the superior surface before it turns upwards as the parietal peritoneum, lining the anterior abdominal wall. Posterior it surrounds the uterus in the female and the rectum in the male. The bladder wall is composed of three layers.
1-) The outer layer of loose connective tissue, containing blood and lymphatic vessels and nerves, covered on the upper surface by the peritoneum.
2-) the middle layer, consisting of interlacing smooth muscle fibres and elastic tissue loosely arranged in three layers. This is called the "detrusor muscle" and when it contracts, it empties the bladder.
3-) the inner mucosa, composed of transitional epithelium that readily permits distension of the bladder as it fills.
The three orifices in the bladder wall form a triangle. The upper two orifices on the posterior wall are the openings of the ureters; The "internal urethral sphincter", a thickening of the urethral smooth muscle layer in the upper part of the urethra, controls outflow of urine from the bladder. This sphincter is not under " voluntary control".
Urethra :
The urethra is a canal extending from the neck of the bladder to the exterior, at the external urethral orifice. It is longer in the male than in the female.
The male urethra is associated with both the urinary and reproductive system.
The female urethra is approximately 4cm long and 6mm in diameter. It runs downwards and forwards behind the synphysis pubis and opens at the "external urethral orifice" just in front of the vagina. The external urethral orifice is guarded by the "external urethral sphincter", which is under voluntary control.
The wall of the female urethra has two main layers: an outer muscle layer and an inner lining of mucosa , which is continuous with that of the bladder. The muscle layer has two parts, an inner layer of smooth muscle that is under autonomic nerve control, and an outer layer of striated muscle surrounding it. The striated muscle forms the external urethral sphincter and is under voluntary control. The mucosa is supported by loose fibroelstic connective tissue containing blood vessels and nerves. Proximally it consists of transitional epithelium while distally it is composed of stratified epithelium.



0 Comments